I saw Dr.Bragg today (how many posts start with/like that?) which was fine, I learned some more info about the upcoming VP Shunt surgery-install.
I have been wondering if the LP Shunt is working optimally, I don't think it's not working just more that based off how i've felt I wonder if the LP Shunt is just not working as well as it should. I am not entirely sure but based off the CT Scan which Dr.Bragg pulled up today the ventricle size is normal (which is a good thing) and should help the VP Shunt placement
be more smooth/precise placement but at the same time my ventricles are never not small except when there's a shunt issue? I definitely don't think it's that the LP Shunt isn't working b/c clearly I'd be a lot sicker and my headaches wouldn't just be intermittent but I think the ventricle size could explain why it seems like my headaches and symptoms are a lot worse? I am not entirely sure, just my feeling..
As far as surgery, my Primary dr. messaged earlier today via MyChart and had not heard back from either of my Cardiology drs. (Cardiologist and Heart Rhythm dr.) yet so she planned to call them again if she'd still not heard anything by the end of today. I honestly am not sure what Dr.Bragg would do if they said either no to surgery or wanted some extra precaution? I pray she'd talk to them to make it a go! Hopefully there just won't be an issue.
In the mean time at today's Appt while looking at the CT Scan results Dr.Bragg talked about what her plan was with this VP Shunt re-replacement. Last time we really talked in depth about this surgery and placement of the distal (draining) end we had agreed b/c of the likely potential an OHS is going to happen to put the 2nd shunt to also drain in to the peritoneum (where the LP Shunt drains).
Today she asked my opinion instead of tunneling this VP Shunt when she places it to drain to the pleural (area around lung) space. She commented if/when we do end up doing the Open heart surgery she realized we'd likely have to go back in and move the shunt distal end but she strongly felt we should maximize the best potential for the most success we could for now and have the 2 shunts drain to separate locations. I was and am happy she thought this and wants to place it in pleural space for now! For all we know a 3rd OHS could be a ways down the road, it seems unlikely given the way my 2 Heart drs talk at each appt. but I would rather have to go back in later and move the distal end temporarily and have better chance of success now with better chance for relief now.
B/c of all the previous pleural space surgeries/procedures and scar tissue she'll get General Surgery involved to do that part of the VP Shunt surgery.. I didn't think to ask her but I wonder how that works, does the shunt get tunneled from the skull, behind the ear, down the chest and then kind of around the side to the pleural space or is there a way they can tunnel it to pleural space from the front? I'll have to ask her at Monday's appt. I am kind of curious.
As far as what ventricle she is going to try to place the distal (top portion of the cathether) in in the brain she said b/c ventricle size is bigger than normal (normal size but bigger than my normal I guess?) she was going to try to place it at the back of my head in the lateral ventricle (I don't know if that's what that ventricle is actually called) as she felt she'd have better success this time then we've had in the past. She also said in prior surgeries they've used a magnetic guidance type system, it's something where there's some sort of sticker (or something) on the forehead and that with the computer I guess helps guide their placement of the shunt catheter?
Anyways instead this time she is going to use a system they use when removing brain tumors, it must be something like they use in c-spine surgeries where your head is held in place by a fixture so it gives her the best chance of best catheter placement within the ventricle (more precise placement, better chance of best outcome I think) while also minimizing/preventing any movement of head during surgery which can throw their computer guided system off.
In any case as long as no hold ups of which I'm still praying every day for there not to be surgery is 2 wks from today. I have to admit this sometimes seems like the surgery that's been a long time coming, a long wait though I am glad we have it scheduled and I know the plan. Dr.Bragg is so awesome about it all even about placing the shunt catheter in to the pleural space for now, knowing it may mean another surgery for that down the road.
I was talking to an MPS Mom just a while ago tonight asking if she might know where I could potentially find the 'MPS I recommended assesments/testing' sheet Genzyme published some yrs ago (it is an elusive fact sheet it seems!) I've asked multiple different Medical People in the MPS Community and at Genzyme and none are entirely aware where to find it but several are helping to try to locate it, so I can send to my Primary dr.
In any case this Mom and I where talking about this sheet and how it would be good to make it available to families again as the information is probably needed - it is important information to know (once I find it/get a copy i'll post it to fb for families) and then she commented something about my having a Team that works together and talks to each other and how she wished she had that for her girls (they are each early 20's), Providers that where willing to work together and communicate as needed.
Honestly I remember just exactly how bad it was in the beginning and all the advice many families gave me. I know how many Specialists I saw and didn't really connect with so I found a different one over time in that Specialty and sometimes it took several different ones before I found one I felt like was a good fit for my care/and team. I also know although it can be a pain how much time I spend driving between where I live and Madison and where I live and Milw. b/c 1/2 my Providers are in Madison including my PCP and the other 1/2 are in Milw. including my weekly ERT Infusion but with this set up my Providers actually communicate with each other.
My PCP does an amazing job talking to other of my Providers when needed and overall my care is really pretty good and especially compared to many in the MPS Community. I get comments frequently from other families on my care Team and how they wish they had Providers like I do. I don't know what the answer to that is but I can say I am grateful for the drs I have albeit it took a lot of time and years to put together who I have on my Team now!
My care now with Providers scattered at 4 different health systems and in Boston (CHW, FMLH, UW-AFCH, UW, and Dean + Dr.Bodamer at BCH in Boston) is amazingly good and frankly much better than it was when all my Specialists where right at CHW and FMLH where each could literally much more easily reach each other. I can't complain to much and I love my Team. =)
I think beyond grateful would be appropriate words to use! God is Good and b/c of him I have great Providers!
Thanks for stopping by,
Erica
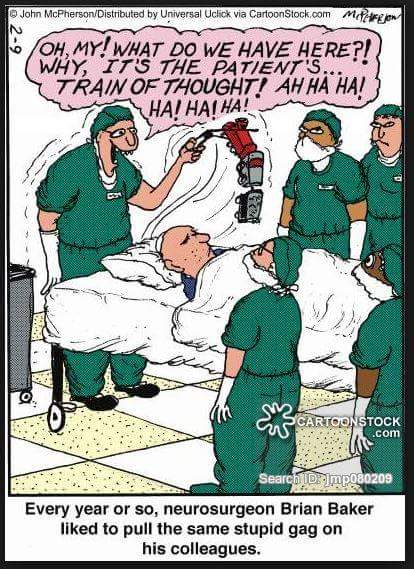
This is not my meme - contrary to some of my typing I can sp 'Operation' =)



It is great that your doctor considered different options before making a decision about surgery.
ReplyDelete