Saw Cardiology today, which I don't always record Appts but days I am overly tired I do. I haven't slept very well in quite a few days which after awhile makes my already, often crap memory worse so these kind of days I do record the appts and then delete once I listen and take notes at home. I have to admit from listening to the 1st Appt and what Dr.Earing emphasized I make sure Dr.Kovach knew to that actual appt with Dr.Kovach and then listening tonight I realized I don't actually think I said much about the symptoms these endless PVCs (skipped or double heart beats) cause. Oops!
I think did an ok or a decent job emphasizing I super hate asking for their help/needing their help and really didn't want to start a new med (we stopped the Beta blocker I was on, wasn't doing much) but with symptoms and the PVCs literally feeling like they are an endless stream-near 75% daily occurrence (maybe not that much but is a ton) I was willing to try something see if we could get under control.
I know I've written and said this before but even though I know the symptoms are very real (and very evident to both Heart drs when they each separately listened) it still makes ya feel a little crazy! Any of this chronic issues stuff does, be it heart, shunts, etc!
It is nice atleast both Heart drs. really work together and try to tag team each other but non-the-less even with really liking both their Nursing Teams and both drs I'd still love to not need them!
But no-less I guess since I do need them I am glad it is the 2 docs I have as I like them both and both seem dedicated and especially keep my whole (bigger MPS) picture in mind!
I couldn't help but think at the appts today, while I am very glad we did the ablation because slowing heart rate has had some impact on both breathing (yay! Isnt perfect but it's somewhat better and I will take that!!) and on how the newest (Mitral) valve seems to be doing so even if we have these issues now with PVCs that are a tad relentless, we'll figure those out! I think the best thing about these 2 (Heart) drs is each will admit when he doesn't know but then they will try to figure it out. Neither gives up either and that with a disorder like my MPS (type I, Hurler Scheie Syndrome) is HUGE! I also can't say what it means as a Patient when your drs really listen and want your opinion and are actually listening to what you have to say.
Re the PVCs as I mentioned above we'll try this Calcium Channel blocker (Verapamil) and say a prayer it works better on these than the CCB class of meds ever did on slowing heart rate! Otherwise if it didn't work/where to con't as bad as it is (I'm thinking positive just listing what I learned) the options aren't all that great. We could try heavier duty arrhythmia meds (but side effects of their own that sound pretty abysmal) or a really last option and 1 we'll try to avoid is doing another ablation to try and capture/deaden where these PVCs are coming from.
-Dr.Kovach did say it's possible a targeted ablation wouldn't be successful either as these could be coming from the L side which is where both my aortic and my mitral mechanical heart valves are and if I remember right isn't possible to target those areas or maybe not easy to target (can't remember exactly).
Concern with another ablation which if it where done would be a 3rd for me (lol 3 OHS, 3 ablations - I think i'll try to avoid tying it up =D ) and much greater risk of permanent damage and again that risk for then needing a permanent pacemaker. Amazingly (but awesomely!) we've come through all 3 Open Heart Surgeries as well as 2 sinus node ablations with no serious damage yet. Wouldn't be bad to keep it at this (no damage, no need for Pacemaker).
A Pacer to would be complicated (?) b/c both of my shunts (LP, VPL) are programmable and dialed to drain a certain amount of CSF. I actually do not know how say the shunts could be re-programmed with out affecting a Pacemaker or vice versa? I'm sure there's some invonvenient way and hopefully we'll never need to find out what that is! =)
Sunday School kids - 1st-2nd, 3rd-4th
Otherwise per Dr.Earing he's hired a newly graduated Adult Congenital Heart doc (Jennifer Girard, MD (sp?) who did her training he said at UofMn and is now finishing up (I think if I remember right) her Adult Congenital Heart fellowship in Atlanta (Emory I'd assume? Will have to ask some friends there if they know her).
Dr.E seems really excited to be setting up a dedicated clinic specific to MPS Pts and our needs and as he put it "a real clinic not just a sort of 1". =) I think he seems to have a interest in these/my MPS disorders which I always think is cool. Given he diagnosed me 12 yrs ago I always appreciative of what he knew and what he's all learned + that he'll admit when he isn't certain (which has been more than a few times in my case) and he'll work to figure out whatever the problem is.
CHW isn't considered an MPS treating center but is a top ranked Congenital Heart Disease treating hospital with superb experience and survival for really tough cases. I think it's perfect there will be another dr. here who is interested in MPS issues and seems to have quite a bit of experience and especially so in Adults with MPS as there are very, very few ACHD Heart drs who are experienced in MPS and/or interested in it!
-I'll end on this - Dr.Kovach's Nurse as we where wrapping up the appt with him (I love his and Dr.Earing's Teams! This Nurse is super sweet) but we where joking about needing a new body and she commented:
"We just worry about you" when she asked me to call and update them in a wk. Funny but very sweet. It means a lot actually when our drs Nurses and for that matter our drs., to, if they care and they can see us as more than just the issue we are there for! =)
I sometimes feel like a pain in the arsh as a Patient (not that I think I am just it's more b/c of needing their help and frankly having to rely on them at times for things 1 would rather not need to rely on people for).
I appreciate when my Providers let me know I am not the bother I often feel like. =)
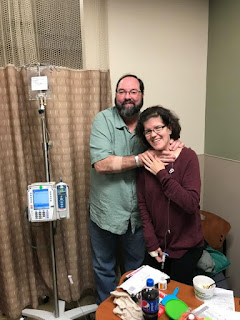
Randy (Fabry dx) and I, we've infused together the majority of my 12yrs
ERT - New Dean Fish Hatchery clinic (start there 16th)
Thanks for stopping by, if there's nothing before I'll update after my 1st infusion in 1.5wks at the Dean-FH site. I finish 1 more infusion under the current (expiring) Prior Auth at FMLH then it's to Madison and the infusion site within my Primary drs. ofc. bldng. She (Dr.Simpson) has asked I have the Nurses page her my 1st day at the new site so she can stop by. Given she really wouldn't have to seems kind of her!Per the Nurse Manager of Dean Infusions there is also 1 specific Nurse assigned to my case. I'm not sure if that's just initially or she'll be my Nurse primarily? Hopefully she (Jill) is nice and to they quickly realize I do my own thing during infusion (calls, paperwork, Sunday School lesson, etc - basically anything I need to get done for the next wk) and non hover to much. =) Dr.Earing was asking if I'd started at the new site yet which I haven't of course and we both agreed (b/c they seem a little nervous? Not sure =) ) as long as nothing with my infusion rate or volume is changed should all go smoothly.
I know when to take the Lasix I already take every day if needed during infusion (if any breathing/coughing symptoms creep up) although that I especially try to avoid (sometimes not possible) but Lasix and infusion = endless bathrm trips. Eeew (I hate public bathrms, lol)!!! Shunts... Ouch!!!
Re Shunt stuff, Dr.Bragg is brainstorming a little for me. She had an interesting idea, given my 1 (Lumbar-thoracic) Shunt causes so much irritation and there is significant scarring and apparently some compression (unsure about this, just what Dr.Iskandar mentioned) maybe see if Dr,Iskandar would take out the LP Shunt and put in 2 VP (from brain) shunts. Don't know that he'll go for it and admittedly I do think as very imperfect as it is when the 2 shunts are working it has been good to have 1 draining from brain (head, VPL Shunt) and 1 draining from my back (Lumbar, low back) Shunt.
While he'll likely say no to this idea I may ask him about this at next appt. I need the 2 shunts but the LP Shunt is wreaking havoc on my spine topped with secondary to my MPS narrowing and compression is already not unusual but the current LP Shunt and prior Spine shunts have caused per Dr.Iskandar severe arachnoiditis (several decompressions to clear scar tissue and remove bone have already been done over the past 5.5-6yrs for this).
Anyways will try to update soon,
Thanks for stopping by,
Erica


No comments:
Post a Comment