Well, wow? What a few days filled with way to much news? Yesterday I saw Cardiology for the 2 week fup, Labs and repeat Echo (ultrasound of the heart). Not the best news. The Echo continues to show increased leaking (perivalvar) around the new mechanical valve and is to the point now where the leaking is severe. Dr.E (Cardiologist) said he could hear the difference even more so while listening to heart beat/rhythm and pulses in wrists/feet where much more palpable as well he had concerns due to my hands being so cold - to that I just said if they would turn the AC down a bit we all might not feel like we where artic frost! Kidding aside this is crappy news and not what I wanted to hear although at the same time I said to him and Nancy (NP) that I also didn't know what to "wish" for? No changes but know they expect there will be worsening as it had continued to and just a matter of when? Or wish for changes but know it would mean having to go back in and do most of the open heart surgery (cracking chest, bi-pass, anesthesia, new healing, etc) again fairly soon (next week already it turns out) but then know at least we would be only a fair amount of weeks away from being able to place the current Thoracic Peritoneal shunt back to it's former (pre-cardiac surgeries) location in the Pleural space? No-win really and not a decision that ultimately no matter was or would have been up to me anyways. I guess I got my "decision" made for me by my body anyways although I admit I was pretty surprised when the CV Surgeon's Secretary called me already Thurs afternoon, not long after I had left the Appt and said they where scheduling it for Tues!? I had tried bartering with Dr.Earing to wait and do the surgery at minimum in mid-Sept (not thinking they would rush it) or even mid-Oct. due to a bunch of stuff going on with Sunday School (planning, a 1-day Conference, meetings/Canvassing, etc.) I think he (Dr.E) just thought that was funny that I wanted to wait as far out as Oct. =/ I thought it seemed like a good plan albeit all the longer we'd have to wait on the shunt business!?
The Aortic Valve replacement-revision is set for Tues., next week, Sept 3rd. The plan is to take out and re-seat the new/leaking valve to get rid of the post-surgery issues or if they feel it would be better they will put in a new mechanical valve and whatever else if anything needs to be done. . What they do depends what they find once I am on bi-pass and opened up. Surgery is scheduled to last from 7:30-1:30.
The Pre-Op Appt which included an Appt w the NP and CV Surgeon's PA, Chest Xray (see that faint glowing, green light in the distance?) and Labs + was to include an EKG. Surgery will be at CHW again and I requested plus was able to get assigned the same Anesthesiologist as last time so that at least is good given she is familiar w my airway now and she was very nice as well very well recommended by my Cardiologist and the Pre-Op NP last time and both where glad she was going to do my case this time.
Did you know that scar tissue at least in heart surgery peaks at week 5/6 post-surgery? I would have guessed if not told that it would be more like 3-6 months post-surgery! This part could make surgery a bit more difficult/longer but they are familiar with my anatomy, I am stopping the Coumadin (blood thinner) as of Sat. and they will have blood on hand if needed. - In the mean time I get to walk around w these very nifty (note sarcasm) white blood product-ID bands all weekend. Yippee! I strongly dislike the feel of these sort of things so am wondering if there might be a way to remove them and re-anchor without being to noticeable. I've not had a chance to look to hard at this yet.
I've heard from numerous Cardiology/Cardiovascular Providers over the past 2 days at Appts how they are amazed at my ability to " just role with the punches" and how so many of their staff comment they like working with me because I never get upset at them for having to give bad news. I am glad actually that people will share this sentiments b/c while I rarely share how I feel about stuff on the outside it does frustrate me that we have to do this again. Not frustrate in a way that I feel it is anyone's fault just more that I feel tired of the MPS sometimes, of so little knowledge about our issues and that when drs do encounter our issues how come there isn't a place they can go and publish or just share that info for the collective good of the MPS community? I know there is Genzyme's Registry but that is only for enrolled providers (typically Genetics I think) and even then it seems few providers share what they see at least mine don't because they don't have time. I wish there was a way for our specialists to share what they see or find in us pts to help other providers? Non-the-less my frustration is calmed a bit (perhaps selfishly) knowing Providers think I am doing an ok job and that they like working with me apparently because I do know like anyone there ARE times I am likely not all peachy and sun-shiny nice and i'd like nothing more than to punch a wall!
Last but not least I saw Dr.Bragg last Thurs for (approx.) 1 month follow up and I can tell she feels bad about the new cardiac issues though she made the comment (purely joking) something to the effect of "I've not worn your parents in to new complications occurring?" - One of the many things I like about her, she can always put a light spin on a crap situation. Her support and her updating her team + the D6-4 Nurses after the last surgery + I imagine this time (she reads/sees my fb) is nice as those Nurses are in a way like another form of family.
And really, truly last! Last night after Church the Pastor (around my age, married w a awefully cute 1 1/2 yr old daughter) invited myself, my Sunday School Co-Teacher and another friend over to his house which was nice. I cant explain it but these are amazing friends and I never have to be anything special around them, they may not totally understand the MPS but both Joan (co-teacher) and Pastor S. are always there to visit in the hospital and Joan and I and another of our Sun. School Teachers have a great time when together either their visiting when I am in-pt, we often do lunch these days after Church when we are all there on Sundays or at our Sunday School meetings. Love them - given I am not much for hanging out with people or going out they really are fun to be around! =)
All for now, since I likely I won't update before Tues's surgery i'll have my Mom update this and fb on Tues and as needed throughout the week. If I am sedated again, if the same plan as last surgery 5 weeks ago is followed Mom will do short updates till I am able again.
Thanks for stopping by,
Erica
"The truth is rarely pure and never simple" (Oscar Wilde). -- This blog reflects my personal life with but not defined by MPS I- reflecting the peaks and valleys of this dx., and my life despite a rare disease while rarely falling within the standard definition of this disorder.
Friday, August 30, 2013
Thursday, August 15, 2013
Cardiology Fup, 3 weeks post-op, Cont'd Valve changes.
Another week (3 weeks post-heart surgery), another Cardiac fup, Labs and Echo. I've come to the conclusion good news doesn't follow me to much atleast medical wise but then I can't say I am ever to surprised. I do believe 'one day at a time' is the best way to handle when you do get bad news, it works for me anyways. I know for others they have other ways of coping and nothing wrong with that either.
This article seems to do a good job of explaining what was done during the Konno Procedure/AVR surgery and what has happened including the "it shouldn't happen in adults" which if nothing else and perhaps sad humor on my part made me laugh (see below).
The good news is I can start cardiac rehab, so the NP is helping get that set up and coordinated. If I do well with this it shows the team I am recovering well and handling the changes to the new valve ok. If I am symptomatic during it gives them a good idea of how to proceed I guess to.
The bad news is the Echo shows the new aortic valve has went from the post-surgery leaks being mild and concerning to the leaks being moderate (change from last weeks Echo to this weeks repeated Echo) at 3 wks post-op. To quote Dr.E "this is more concerning" as well as "disappointing" but they'll con't to watch closely, keeping pre-AVR meds the same for now and repeat the Echo again in 2 weeks with fup after. If no changes we likely would not have to do anything w the new valve but con't to watch it but if it continues to worsen then we would have to go back in and replace this aortic valve with a new one meaning another open heart surgery, balancing the steroids, anesthesia, etc. The upside of a downside to that would be we wouldn't have to repeat the aortic root enlargement (konno procedure) which made this last OHS that much longer and more complicated. I'd really like to not have to do anything heart related! They know the leaks are coming from the aortic root enlargement and subsequent patch and believe a stitch/stitches have come loose leading to the leaking. Had they not enlarged this aortic root and annulus they would have had to use a pediatric size valve though which in turn would have posed it's own issues and would have been more likely to cause less overall success with the surgery and heart long-term. I just would hope this settles out soon enough as i'd really like for there not to be a delay in our being able to place the Thoracic shunt back in to the pleural space sooner rather than later (8-12 wks post-op per Cardiology)! Not that I want any surgery but that shunt draining elsewhere makes a significant difference. I fup w Dr.Bragg, Neurosurgery next week so will be curious what she has to say.
Today's labs show the Coumadin level cont's to be to low so this was adjusted from 4mgs 5 days a week and 6mgs 2 days a week to 6 mgs 5 days a week and 4 mgs 2 days a week with repeat INR again before the fup Appt in 2 weeks.
Dr.E said to me today something along the lines of "if it was going to happen to someone I guess I am not surprised it was you", meaning w the MPS and other surgeries i've sailed through many-a surgeries only then to have complications afterward (shunts for instance). Probably isn't funny and he didn't really mean it to be but in the face of bad news that statement kind of made me laugh. What else are ya going to do, right? Not worth stressing over to me as to much can change in an instant anyways. He did say given how worried he was before the heart surgery and my being high-risk + how hard he thought the surgery/post-op would be that he was happy I sailed through this post-op and recovery as well as I did! I agree!! He has admitted he's disappointed and worried, I figure i'll leave that to him (and my Mom whom I know this drives crazy) and like I said above I figure I can't change it anyways so it is in God's hands and i'll worry about what I can influence ie other things. =)
On a side note we had our 2nd (my first) Sunday School meeting of the year, planning the 1st day (we are going to do a group-all classes activity one sunday a month vs every sunday in our individual classrooms) as well as going over our information for canvassing in a few wks which just means passing out flyers/brochures related to SS. Last we went over a bit of the SS Conference in mid-Sept. After a long afternoon in Milw I was already tired but still a good meeting.
Thanks for stopping by,
Erica
This article seems to do a good job of explaining what was done during the Konno Procedure/AVR surgery and what has happened including the "it shouldn't happen in adults" which if nothing else and perhaps sad humor on my part made me laugh (see below).
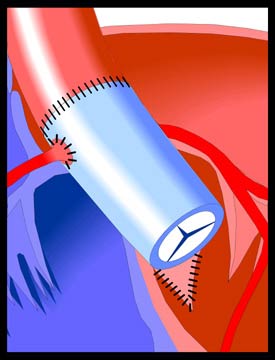 | Aortic Stenosis - Konno Procedure This procedure is performed in cases of Aortic Stenosis when the left ventricular outflow tract is stenotic in addition to the aortic valve itself. It involves the replacement of the aortic valve and the widening of the ventricular septum in the region of the valve with a patch (see illustration). The aortic valve is replaced with either a mechanical valve (Konno-Rastan Procedure), an aortic homograft (human aortic valve), or with the patient's own pulmonary valve. In the last case, the valve may grow and renew itself over time. However, the first two types of replacement valve will eventually need to be replaced as the function over time decreases. After the Konno Procedure, the possibility of renewed narrowing of the left ventricular outflow tract (LVOT) exists and the patient will need regular monitoring. The development of a new systolic murmur or the intensification of a soft murmur is an indication that the LVOT should be investigated through echocardiography. The aortic valve itself also needs to be monitored to guard against progressive aortic insufficiency. If this becomes significant, reoperation will be necessary. However, significant aortic insufficiency is uncommon in the adult patient and mild insufficiency is well-tolerated and generally remains stable for long periods. Most surgically implanted mechanical valves will last 10-20 years before they wear out, become obstructed, or lose efficiency. When their function becomes impaired for any of these reasons, replacement becomes necessary |
The good news is I can start cardiac rehab, so the NP is helping get that set up and coordinated. If I do well with this it shows the team I am recovering well and handling the changes to the new valve ok. If I am symptomatic during it gives them a good idea of how to proceed I guess to.
The bad news is the Echo shows the new aortic valve has went from the post-surgery leaks being mild and concerning to the leaks being moderate (change from last weeks Echo to this weeks repeated Echo) at 3 wks post-op. To quote Dr.E "this is more concerning" as well as "disappointing" but they'll con't to watch closely, keeping pre-AVR meds the same for now and repeat the Echo again in 2 weeks with fup after. If no changes we likely would not have to do anything w the new valve but con't to watch it but if it continues to worsen then we would have to go back in and replace this aortic valve with a new one meaning another open heart surgery, balancing the steroids, anesthesia, etc. The upside of a downside to that would be we wouldn't have to repeat the aortic root enlargement (konno procedure) which made this last OHS that much longer and more complicated. I'd really like to not have to do anything heart related! They know the leaks are coming from the aortic root enlargement and subsequent patch and believe a stitch/stitches have come loose leading to the leaking. Had they not enlarged this aortic root and annulus they would have had to use a pediatric size valve though which in turn would have posed it's own issues and would have been more likely to cause less overall success with the surgery and heart long-term. I just would hope this settles out soon enough as i'd really like for there not to be a delay in our being able to place the Thoracic shunt back in to the pleural space sooner rather than later (8-12 wks post-op per Cardiology)! Not that I want any surgery but that shunt draining elsewhere makes a significant difference. I fup w Dr.Bragg, Neurosurgery next week so will be curious what she has to say.
Today's labs show the Coumadin level cont's to be to low so this was adjusted from 4mgs 5 days a week and 6mgs 2 days a week to 6 mgs 5 days a week and 4 mgs 2 days a week with repeat INR again before the fup Appt in 2 weeks.
Dr.E said to me today something along the lines of "if it was going to happen to someone I guess I am not surprised it was you", meaning w the MPS and other surgeries i've sailed through many-a surgeries only then to have complications afterward (shunts for instance). Probably isn't funny and he didn't really mean it to be but in the face of bad news that statement kind of made me laugh. What else are ya going to do, right? Not worth stressing over to me as to much can change in an instant anyways. He did say given how worried he was before the heart surgery and my being high-risk + how hard he thought the surgery/post-op would be that he was happy I sailed through this post-op and recovery as well as I did! I agree!! He has admitted he's disappointed and worried, I figure i'll leave that to him (and my Mom whom I know this drives crazy) and like I said above I figure I can't change it anyways so it is in God's hands and i'll worry about what I can influence ie other things. =)
On a side note we had our 2nd (my first) Sunday School meeting of the year, planning the 1st day (we are going to do a group-all classes activity one sunday a month vs every sunday in our individual classrooms) as well as going over our information for canvassing in a few wks which just means passing out flyers/brochures related to SS. Last we went over a bit of the SS Conference in mid-Sept. After a long afternoon in Milw I was already tired but still a good meeting.
Thanks for stopping by,
Erica
Wednesday, August 7, 2013
Cardiology Fup update, An Anesthesia Provider-Summary option
Yesterday was the 1st fup with the Cardiology Team since I got released last Friday including Labs, Xray, repeat Echo (3rd regular one since the surgery) and fup w the Cardiologist. All seems to con't to be going ok with the new post-surgery VSD and 2 aortic valve leaks being stable and INR (blood thinner level) was just a little low so that med dose was adjusted accordingly. Their main worry cont's it seems to be is there a infection (bacterial endocarditis) but I have no symptoms of this so I think they just are watching closely to be sure.
The next follow up appt will continue to be in 1 week with Labs and repeat Echo followed by seeing the Cardiologist again. Otherwise the only change was to the dose of Coumadin as level was somewhat to low, this just went up to 6mgs 2 days a week and 4mgs 5 days a week. This level going up and down isn't that unusual in the beginning as ones body adjusts to the med and blood levels being thinned.
Otherwise i've had to change around a few appts because of these Cardiology fups with seeing Pain Mngmt dr next week and then Neurosurgery the following week. We have to wait 8-12 weeks to replace the Thoracic shunt back in to the pleural space but Dr.Bragg had wanted a fup appt about a month after I last saw her or when I was feeling well enough from the heart surgery. I think one she may want to check the shunt settings (?) and 2 I imagine we'll begin to look at placing the shunt back ie a timeframe and plan which I imagine will be sometime in Oct. though not certain. Otherwise just kind of bored and looking fwd to being able to drive again!!!!
Below I've posted a summary letter I received from the Anesthesiologist at CHW who did the heart surgery and the TEE as she emailed me this the other day as a means for future new providers/surgeries to be aware of what they will be dealing with. I only rarely post this kind of thing but have been thinking about this and really think it is a good example of something MPS Families/Adults might want to consider requesting from their Anesthesiologist as it can be helpful, is well laid out and explains all airway issues this dr ran in to very well. As I think I posted in one of the previous updates this dr commented to me how un-helpful the actual Anesthesiol. notes from UW where in preparing her for what she would see and so she asked me if writing something like this would be helpful in order for future, new drs to not minimize the issues ahead of time. I will leave the providers full name off the end.
August 3, 2013
The next follow up appt will continue to be in 1 week with Labs and repeat Echo followed by seeing the Cardiologist again. Otherwise the only change was to the dose of Coumadin as level was somewhat to low, this just went up to 6mgs 2 days a week and 4mgs 5 days a week. This level going up and down isn't that unusual in the beginning as ones body adjusts to the med and blood levels being thinned.
Otherwise i've had to change around a few appts because of these Cardiology fups with seeing Pain Mngmt dr next week and then Neurosurgery the following week. We have to wait 8-12 weeks to replace the Thoracic shunt back in to the pleural space but Dr.Bragg had wanted a fup appt about a month after I last saw her or when I was feeling well enough from the heart surgery. I think one she may want to check the shunt settings (?) and 2 I imagine we'll begin to look at placing the shunt back ie a timeframe and plan which I imagine will be sometime in Oct. though not certain. Otherwise just kind of bored and looking fwd to being able to drive again!!!!
Below I've posted a summary letter I received from the Anesthesiologist at CHW who did the heart surgery and the TEE as she emailed me this the other day as a means for future new providers/surgeries to be aware of what they will be dealing with. I only rarely post this kind of thing but have been thinking about this and really think it is a good example of something MPS Families/Adults might want to consider requesting from their Anesthesiologist as it can be helpful, is well laid out and explains all airway issues this dr ran in to very well. As I think I posted in one of the previous updates this dr commented to me how un-helpful the actual Anesthesiol. notes from UW where in preparing her for what she would see and so she asked me if writing something like this would be helpful in order for future, new drs to not minimize the issues ahead of time. I will leave the providers full name off the end.
August 3, 2013
To Whom It May Concern:
Last month, I had thAuguste pleasure of providing anesthesia to Erica Thiel for aortic valve replacemen and subsequent TEE prior to her discharge. As you are aware, she has Hurler Scheie type 1, which is commonly associated with airway challenges during anesthesia, becoming progressively worse as the patient gets older.
Erica has a number of features on physical examination that suggest intubation may be challenging: limited extension of the cervical spine due to her disease as well as cervical fusion from C2-4; variable degree of mouth opening, and Mallampati III. However she has normal jaw contour and generous thyromental distance.
Her face is somewhat narrow and the #4 mask provides a much better fit than does the #5 adult mask. She is easily ventilated by mask with or without muscle relaxation.
It should not come as a surprise that direct laryngoscopy was not successful. The Macintosh #3 blade would not advance to the base of the tongue. A glidescope provided visualization of the posterior aspect of her larynx and vocal cords but I was not able to advance the endotracheal tube into the hypopharynx due to her small mouth size and limited opening under anesthesia. Nasal fiberoptic intubation was successful after dilation with 26 and 28 nasopharyngeal airways, although the insertion of same resulted in nasopharyngeal bleeding. In addition, once anesthetized, she had copious oral secretions.
Following her aortic valve replacement, she remained intubated to avoid potential airway difficulties in the setting of emergency return to the operating room for bleeding or other surgical complications.
She underwent TEE prior to discharge, and tolerated the procedure well. She was progressively sedated with midazolam, fentanyl and ketamine without any airway challenges throughout the case.
She has adrenal insufficiency and thought that perhaps her dizziness and strange sensation following the procedure might have been due to the lack of a stress dose of steroids, which I did not administer because I did not think that the echocardiogram would be sufficiently stressful to her physiology.
Erica is keenly aware of her medical issues and deals with them quite effectively. She has requested that I provider her with this information hoping that it may be useful to other providers who are unfamiliar with her history.
Sincerely,
Thanks for stopping by,
Erica
Saturday, August 3, 2013
Discharged day 10, Out of the Hospital!!
Friday, I got discharged and released today!! 2 of my co-sunday school teachers had actually come to visit Friday and so they hung out while all the various specialists filed through, all the discharge paperwork was done and while last minute things where ironed out + the fup appts scheduled. After that we just had to stop at the Skywalk Pharmacy and where home-ward bound!! We stopped to get ice cream and otherwise was a really nice drive back as these 2 are pretty funny and mostly I just listened but they definitely know how to make you laugh. =) For fup Appts.Tuesday I have to fup in Cardiology with a Lab tests, Xray(s), repeat Echo (3rd in a week) and an Appt with the Cardiologist to make sure there are no changes in the 2 leaks and the 1 hole as well as to make sure the Coumadin levels are staying pretty stable.
I slept from around 11 Friday night till almost 12-noon on Sat morning with waking up a couple times but quickly falling back asleep. Wow! I am tired today but in that "probably need one more good night to catch up" way so if I sleep well tonight I should be pretty well caught up tomorrow!
Sat - The Anesthestiologist who did my Open Heart Surgery and the TEE emailed me earlier this afternoon and included her summary letter/thoughts on her findings during both the OHS and the TEE plus what she used, what she found per what she initially thought, what she recommends to future Anesthesiologists and her thought that to we need to do pre-procedure stress-dosing as she commented on my thoughts that I thought the post-TEE symptoms where adrenal crisis related. She listed why she had not used them but said she would recommend it be done in the future. My Neuro-Endocrine dr did say after the TEE when I messaged her that the cortisol should be done for every surgery and every procedure (same as she has said in the past but like I said we all just got busy and was kind of a last min procedure) if ANY kind of sedation used so I am glad Dr.Taylor made that addt'l comment. :) It is definitely well written so I am glad to have it!
Otherwise I am happy to be home, have been working on a project for the Foundation I work for an in addition catching up on paperwork and information from our recent, 1st of the year Sunday School meeting (and information on a 1 day Conf in Sept our SS Teachers are attending in Madison with other WELS SS Teachers, hosted by Northwestern Publishing House) + just kind of taking it easy other than having run over to my Apt in Juneau to get my car (my Dad drove it back) while my Mom and I got a few things and afterwards went to the store. Healing cont's to be ok, I am not to terribly sore and definitely not as bad (as ive said before) as the various spine surgeries-maybe bc those included hardware? With OHS you are In an area that has far less nerves though so the wires to pull the sternum back together make it uncomfortable but not anywhere what I thought it would be. Swallowing (painful in upper chest/lower esophagus) is also seeming get a slight, bit better. =) For now I just eat small amounts of softer foods.
Will update if nothing else after Monday's ERT/Tuesday's Cardiology Appts.
Thanks for stopping by,
Erica
I slept from around 11 Friday night till almost 12-noon on Sat morning with waking up a couple times but quickly falling back asleep. Wow! I am tired today but in that "probably need one more good night to catch up" way so if I sleep well tonight I should be pretty well caught up tomorrow!
Sat - The Anesthestiologist who did my Open Heart Surgery and the TEE emailed me earlier this afternoon and included her summary letter/thoughts on her findings during both the OHS and the TEE plus what she used, what she found per what she initially thought, what she recommends to future Anesthesiologists and her thought that to we need to do pre-procedure stress-dosing as she commented on my thoughts that I thought the post-TEE symptoms where adrenal crisis related. She listed why she had not used them but said she would recommend it be done in the future. My Neuro-Endocrine dr did say after the TEE when I messaged her that the cortisol should be done for every surgery and every procedure (same as she has said in the past but like I said we all just got busy and was kind of a last min procedure) if ANY kind of sedation used so I am glad Dr.Taylor made that addt'l comment. :) It is definitely well written so I am glad to have it!
Otherwise I am happy to be home, have been working on a project for the Foundation I work for an in addition catching up on paperwork and information from our recent, 1st of the year Sunday School meeting (and information on a 1 day Conf in Sept our SS Teachers are attending in Madison with other WELS SS Teachers, hosted by Northwestern Publishing House) + just kind of taking it easy other than having run over to my Apt in Juneau to get my car (my Dad drove it back) while my Mom and I got a few things and afterwards went to the store. Healing cont's to be ok, I am not to terribly sore and definitely not as bad (as ive said before) as the various spine surgeries-maybe bc those included hardware? With OHS you are In an area that has far less nerves though so the wires to pull the sternum back together make it uncomfortable but not anywhere what I thought it would be. Swallowing (painful in upper chest/lower esophagus) is also seeming get a slight, bit better. =) For now I just eat small amounts of softer foods.
Will update if nothing else after Monday's ERT/Tuesday's Cardiology Appts.
Thanks for stopping by,
Erica
Thursday, August 1, 2013
Trans-Thoracic Echo, Echo (heart) changes. Past several days post-op.
So we did a "going home" Echo yesterday (Tues) and one of those tests you can tell as they are doing it that something isn't right. Not only did it take double as long (2 hrs) but they had the head-Echo dr in here and then my Cardiologist both reviewing the images and repeating different and new frames. I was so tired I just didn't care admittedly. Not long after that the NP for my Cardiologist came past the room and asked "Dr.E wants to know the last time you've eaten or dranken anything?" - Ding, ding.. Always a give away that they they are wanting to do something with some form of sedation. About 30mins after that my Cardiologist came by and told me they found what they felt was 2 new leaks and maybe a hole on the earlier Echo (leaking) that where not there before surgery or on the post-surgery TEE and he wanted to do a trans-thoracic Echo that afternoon at 2 and had already lined up the Anesthesiologist I had the previous week so she was intimately familiar with my airway and how best to handle this during the Trans-Echo (aka TEE). These Trans-Echo results showed 2 small leaks in the new aortic valve and a hole between the newly enlarged and patched aortic root and either the new valve or another part of the heart; I cant fully remember that part. For now they will since all new issues are small will just repeat a regular (non-TEE) Echo on Thurs and and follow my case much more closely than they otherwise would have to make sure there isn't 1. Bacterial Endocarditis forming (no symptoms of this) or 2. the Hole and leaking don't get worse as if those did they would likely have to go back via the Cath Lab or open heart (cath lab I think) to repair these areas which would be a big deal apparently.
Repeat Echo today (Thurs) showed no change in the 3 new issues and so if blood lab cultures run yesterday come back negative I can get sprung!! Dr.Earing did say I'll have to f/up with him on a weekly basis for awhile to monitor the 2 new leaks and 1 new hole for possible changes or symptoms but otherwise would be home sweet home! I really don't know what the schedule is for Coumadin-lab checks initially. I imagine they go over that info in discharge paperwork. Sutures came out of the 3 chest tube sites this morning and the steri-strips along the sternum chest incision will fall off on their own. The stitches are internal and dissolvable + the wires stay in place and help the broken bone heal, typically in about a 2 month process.
Ironically yesterday (Tues, day of the TEE) morning I had been feeling really great, the complete best in the past week which was actually saying a lot as I hadn't felt too terrible most of the previous few days. I managed to wash my hair myself while semi-leaning over the shower/holding on to the railing and had gotten washed up + dressed + was working with PT. I had walked the halls, I was feeling raring to go! Post-TEE? Not so much, even today a day later I feel like a truck has ran me over both tired and achy wise. With PT I did manage to take a regular shower this morning though and dressed in semi-regular clothes + then took a nap this morning and this afternoon. On a separate note the Cardiothoracic Resident did say I should be able to drive within 1-2 weeks given how well I am doing recovery wise!! Even with this set-backs I think I am surpassing anyone's expectation for my recovery time and even many otherwise healthy open heart pts recovery times. =)
One thing we did forget with the sedation and procedure (TEE) yesterday was to give pre-sedation cortisol replacement dosing and so that likely explains why I had such a terrible post-OR recovery and feel so washed out/drained today. A mistake I won't make again! The cortisol literally acts as the rescue-stress hormones I don't make and helps the body handle stress like sedation/anesthesia, procedures and recovery ability. Yikes, that was pretty aweful crap!!!! I didn't realize it was the cortisol replacement until later Tues night when I was starting to feel slightly more normal and thinking over what could have possibly caused the post-procedure to go so terrible. It finally occurred to me we hadn't given that med in the last min decision to do the procedure and last minute planning.
Definitely something I wont forget even in last minute procedures in the future!
In talking to the Cardiothoracic Resident the other day I asked him what his general experience is with people being able to drive post-op and he said he was fairly certain with how well I am doing I should be able to drive in a couple weeks! AWESOME!! That was some of the best news I could have heard! I am on a 5pd/each hand, 10 pd total weight restriction for 2 months so I will have to have my Dad come over periodically when I do go back home, probably in a few weeks and help me stock up on cat food and cat litter and put these in to large Tupperware containers I can then just scoop out of. =)
On a completely different note I had the same Anesthesiologist as last week and we where talking about what she all used/did differently to get me intubated ("the whole toolbox") and she asked me if I would like her to write a summary of her findings, what she used, and recommends! This was while in pre-op holding for the TEE and as they where getting everything ready in the OR so I didn't ask her how best to get this from her when she has it completed but the Resident paged her just before to ask for me. She commented how my upper airway (throat) is really pretty almost easy to work with but when she got to lower airway or a little further down she said the various Anesthesiologists notes I had given her from UW in no way prepared her for what she was working with and she couldn't emphasize enough that in the future with new Anesthesiologists I needed to not minimize in any way how bad the airway is (they felt if they had taken out the ventilator support to soon they likely wouldn't have been able to get an airway support back in and would have to do a Trach.) She just said how blown away really she was by my features given how 'mild' I look in appearance and yet how difficult of a time she had getting the airway intubated, to use her words "I had to pull out the whole arsenal in your case".
This whole week we've spent trying to get Genetics to get the Aldurazyme over here or order it (given we can get it at UW there is NO reason they couldn't have gotten the drug!!!!). Needless to say initially they told my Cardiology team that I could skip a week since I was a week out from a big surgery (read that again A WEEK OUT!) so they weren't going to order it. My Cardiologist initially sided with them but once I explained quite frankly why I felt they where saying that he began to try and help get the drug. I fought back on this issue and talked to my Insurance Nurse Case Man. who said we could have the drug over-nighted (what we frequently do at UW) and so I passed that message to my GC. Do you think she ordered it Tues? Nope! Weds comes and finally they have decided they will order it but did not have it over-nighted (sooo dysfunctional of a clinic!!!!) and so if it got here Weds I would get it and get infused Mon at normal time yet. No drug yesterday. So today we are waiting for it and unsure if I will get it or not as I would then miss Monday's regular dose. Grr!!! Why if UW can do this couldn't Genetics have had me sign a waiver to use MY OWN DRUG in their ofc 50 feet away or over-night ordered Monday or Tues? I have a 4 letter (non-explicit) word that starts w an L that says why. =/
One of my ERT Infusion Nurses has visited everyday with her co-workers, a different one each day (all whom I have gotten to know, the one is married to the Head of Peds Neurosurgery here at CHW and who grilled me almost 2 yrs ago about Dr.Bragg, not bc she didn't trust her but bc she wanted to make sure I was getting great care.) =) Anyways so they where telling me that last week when I was still intubated and sedated over those 3 days I would frequently try to sit up and mouth "my head hurts" while trying to hold my head. I was actually a little amazed by this but grateful they told me as it validates that I do in fact get the positional headaches and not just in my head (per se)! I completely know Dr.Bragg has always believed me but you still can't help but question yourself sometimes!
So far we are just waiting for blood cultures today to see if I get to go home or not, is day 10 post-heart surgery so not to bad but still will be happy to go home! I can deal with all the post-op fups if it It means my own comforts at home or as is for now at my parents. =)
Thanks for stopping by,
Erica
Repeat Echo today (Thurs) showed no change in the 3 new issues and so if blood lab cultures run yesterday come back negative I can get sprung!! Dr.Earing did say I'll have to f/up with him on a weekly basis for awhile to monitor the 2 new leaks and 1 new hole for possible changes or symptoms but otherwise would be home sweet home! I really don't know what the schedule is for Coumadin-lab checks initially. I imagine they go over that info in discharge paperwork. Sutures came out of the 3 chest tube sites this morning and the steri-strips along the sternum chest incision will fall off on their own. The stitches are internal and dissolvable + the wires stay in place and help the broken bone heal, typically in about a 2 month process.
Ironically yesterday (Tues, day of the TEE) morning I had been feeling really great, the complete best in the past week which was actually saying a lot as I hadn't felt too terrible most of the previous few days. I managed to wash my hair myself while semi-leaning over the shower/holding on to the railing and had gotten washed up + dressed + was working with PT. I had walked the halls, I was feeling raring to go! Post-TEE? Not so much, even today a day later I feel like a truck has ran me over both tired and achy wise. With PT I did manage to take a regular shower this morning though and dressed in semi-regular clothes + then took a nap this morning and this afternoon. On a separate note the Cardiothoracic Resident did say I should be able to drive within 1-2 weeks given how well I am doing recovery wise!! Even with this set-backs I think I am surpassing anyone's expectation for my recovery time and even many otherwise healthy open heart pts recovery times. =)
One thing we did forget with the sedation and procedure (TEE) yesterday was to give pre-sedation cortisol replacement dosing and so that likely explains why I had such a terrible post-OR recovery and feel so washed out/drained today. A mistake I won't make again! The cortisol literally acts as the rescue-stress hormones I don't make and helps the body handle stress like sedation/anesthesia, procedures and recovery ability. Yikes, that was pretty aweful crap!!!! I didn't realize it was the cortisol replacement until later Tues night when I was starting to feel slightly more normal and thinking over what could have possibly caused the post-procedure to go so terrible. It finally occurred to me we hadn't given that med in the last min decision to do the procedure and last minute planning.
Definitely something I wont forget even in last minute procedures in the future!
In talking to the Cardiothoracic Resident the other day I asked him what his general experience is with people being able to drive post-op and he said he was fairly certain with how well I am doing I should be able to drive in a couple weeks! AWESOME!! That was some of the best news I could have heard! I am on a 5pd/each hand, 10 pd total weight restriction for 2 months so I will have to have my Dad come over periodically when I do go back home, probably in a few weeks and help me stock up on cat food and cat litter and put these in to large Tupperware containers I can then just scoop out of. =)
On a completely different note I had the same Anesthesiologist as last week and we where talking about what she all used/did differently to get me intubated ("the whole toolbox") and she asked me if I would like her to write a summary of her findings, what she used, and recommends! This was while in pre-op holding for the TEE and as they where getting everything ready in the OR so I didn't ask her how best to get this from her when she has it completed but the Resident paged her just before to ask for me. She commented how my upper airway (throat) is really pretty almost easy to work with but when she got to lower airway or a little further down she said the various Anesthesiologists notes I had given her from UW in no way prepared her for what she was working with and she couldn't emphasize enough that in the future with new Anesthesiologists I needed to not minimize in any way how bad the airway is (they felt if they had taken out the ventilator support to soon they likely wouldn't have been able to get an airway support back in and would have to do a Trach.) She just said how blown away really she was by my features given how 'mild' I look in appearance and yet how difficult of a time she had getting the airway intubated, to use her words "I had to pull out the whole arsenal in your case".
This whole week we've spent trying to get Genetics to get the Aldurazyme over here or order it (given we can get it at UW there is NO reason they couldn't have gotten the drug!!!!). Needless to say initially they told my Cardiology team that I could skip a week since I was a week out from a big surgery (read that again A WEEK OUT!) so they weren't going to order it. My Cardiologist initially sided with them but once I explained quite frankly why I felt they where saying that he began to try and help get the drug. I fought back on this issue and talked to my Insurance Nurse Case Man. who said we could have the drug over-nighted (what we frequently do at UW) and so I passed that message to my GC. Do you think she ordered it Tues? Nope! Weds comes and finally they have decided they will order it but did not have it over-nighted (sooo dysfunctional of a clinic!!!!) and so if it got here Weds I would get it and get infused Mon at normal time yet. No drug yesterday. So today we are waiting for it and unsure if I will get it or not as I would then miss Monday's regular dose. Grr!!! Why if UW can do this couldn't Genetics have had me sign a waiver to use MY OWN DRUG in their ofc 50 feet away or over-night ordered Monday or Tues? I have a 4 letter (non-explicit) word that starts w an L that says why. =/
One of my ERT Infusion Nurses has visited everyday with her co-workers, a different one each day (all whom I have gotten to know, the one is married to the Head of Peds Neurosurgery here at CHW and who grilled me almost 2 yrs ago about Dr.Bragg, not bc she didn't trust her but bc she wanted to make sure I was getting great care.) =) Anyways so they where telling me that last week when I was still intubated and sedated over those 3 days I would frequently try to sit up and mouth "my head hurts" while trying to hold my head. I was actually a little amazed by this but grateful they told me as it validates that I do in fact get the positional headaches and not just in my head (per se)! I completely know Dr.Bragg has always believed me but you still can't help but question yourself sometimes!
So far we are just waiting for blood cultures today to see if I get to go home or not, is day 10 post-heart surgery so not to bad but still will be happy to go home! I can deal with all the post-op fups if it It means my own comforts at home or as is for now at my parents. =)
Thanks for stopping by,
Erica
Subscribe to:
Posts (Atom)