This article seems to do a good job of explaining what was done during the Konno Procedure/AVR surgery and what has happened including the "it shouldn't happen in adults" which if nothing else and perhaps sad humor on my part made me laugh (see below).
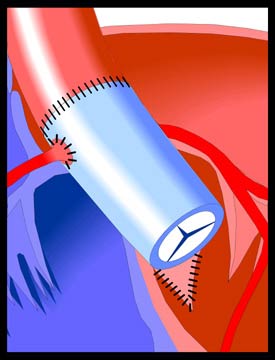 | Aortic Stenosis - Konno Procedure This procedure is performed in cases of Aortic Stenosis when the left ventricular outflow tract is stenotic in addition to the aortic valve itself. It involves the replacement of the aortic valve and the widening of the ventricular septum in the region of the valve with a patch (see illustration). The aortic valve is replaced with either a mechanical valve (Konno-Rastan Procedure), an aortic homograft (human aortic valve), or with the patient's own pulmonary valve. In the last case, the valve may grow and renew itself over time. However, the first two types of replacement valve will eventually need to be replaced as the function over time decreases. After the Konno Procedure, the possibility of renewed narrowing of the left ventricular outflow tract (LVOT) exists and the patient will need regular monitoring. The development of a new systolic murmur or the intensification of a soft murmur is an indication that the LVOT should be investigated through echocardiography. The aortic valve itself also needs to be monitored to guard against progressive aortic insufficiency. If this becomes significant, reoperation will be necessary. However, significant aortic insufficiency is uncommon in the adult patient and mild insufficiency is well-tolerated and generally remains stable for long periods. Most surgically implanted mechanical valves will last 10-20 years before they wear out, become obstructed, or lose efficiency. When their function becomes impaired for any of these reasons, replacement becomes necessary |
The good news is I can start cardiac rehab, so the NP is helping get that set up and coordinated. If I do well with this it shows the team I am recovering well and handling the changes to the new valve ok. If I am symptomatic during it gives them a good idea of how to proceed I guess to.
The bad news is the Echo shows the new aortic valve has went from the post-surgery leaks being mild and concerning to the leaks being moderate (change from last weeks Echo to this weeks repeated Echo) at 3 wks post-op. To quote Dr.E "this is more concerning" as well as "disappointing" but they'll con't to watch closely, keeping pre-AVR meds the same for now and repeat the Echo again in 2 weeks with fup after. If no changes we likely would not have to do anything w the new valve but con't to watch it but if it continues to worsen then we would have to go back in and replace this aortic valve with a new one meaning another open heart surgery, balancing the steroids, anesthesia, etc. The upside of a downside to that would be we wouldn't have to repeat the aortic root enlargement (konno procedure) which made this last OHS that much longer and more complicated. I'd really like to not have to do anything heart related! They know the leaks are coming from the aortic root enlargement and subsequent patch and believe a stitch/stitches have come loose leading to the leaking. Had they not enlarged this aortic root and annulus they would have had to use a pediatric size valve though which in turn would have posed it's own issues and would have been more likely to cause less overall success with the surgery and heart long-term. I just would hope this settles out soon enough as i'd really like for there not to be a delay in our being able to place the Thoracic shunt back in to the pleural space sooner rather than later (8-12 wks post-op per Cardiology)! Not that I want any surgery but that shunt draining elsewhere makes a significant difference. I fup w Dr.Bragg, Neurosurgery next week so will be curious what she has to say.
Today's labs show the Coumadin level cont's to be to low so this was adjusted from 4mgs 5 days a week and 6mgs 2 days a week to 6 mgs 5 days a week and 4 mgs 2 days a week with repeat INR again before the fup Appt in 2 weeks.
Dr.E said to me today something along the lines of "if it was going to happen to someone I guess I am not surprised it was you", meaning w the MPS and other surgeries i've sailed through many-a surgeries only then to have complications afterward (shunts for instance). Probably isn't funny and he didn't really mean it to be but in the face of bad news that statement kind of made me laugh. What else are ya going to do, right? Not worth stressing over to me as to much can change in an instant anyways. He did say given how worried he was before the heart surgery and my being high-risk + how hard he thought the surgery/post-op would be that he was happy I sailed through this post-op and recovery as well as I did! I agree!! He has admitted he's disappointed and worried, I figure i'll leave that to him (and my Mom whom I know this drives crazy) and like I said above I figure I can't change it anyways so it is in God's hands and i'll worry about what I can influence ie other things. =)
On a side note we had our 2nd (my first) Sunday School meeting of the year, planning the 1st day (we are going to do a group-all classes activity one sunday a month vs every sunday in our individual classrooms) as well as going over our information for canvassing in a few wks which just means passing out flyers/brochures related to SS. Last we went over a bit of the SS Conference in mid-Sept. After a long afternoon in Milw I was already tired but still a good meeting.
Thanks for stopping by,
Erica
No comments:
Post a Comment